In a study published on December 10, 2021 in The Lancet Oncology, Prof J. Zucman-Rossi’s team at the Cordeliers Research Centre (Université Paris Cité, Sorbonne University, Inserm) and collaborators from the GENTHEP network, identified two new genes; WNT3A-WNT9A, which certain genetic variations are associated with the risk of developing hepatocellular carcinoma in patients with chronic heavy alcohol consumption. These findings provide a better understanding of interaction mechanisms as a consequence of lifelong exposure to alcohol and the genetic diversity of alcohol-drinkers leading to the development of liver cancer.
Hepatocellular carcinoma (HCC) is the most common cause of liver malignancy and the third most common cause of cancer-related death worldwide. In France and in many Western countries, alcohol consumption of more than 4 glasses per day is the main driver of HCC.
Although the risk of developing liver cancer increases with the severity of alcohol-related liver damage, liver cancer will only develop within a subset of long-term alcohol users. This finding suggests that genetic factors are involved in the development of HCC on the background of alcohol-related liver disease. Understanding why some patients develop alcohol-related HCC and others do not, is the question that was asked by the team of Prof. Jessica Zucman-Rossi at the Cordeliers Research Center, and by her collaborators of the Genetic Network of Liver Tumors (GENTHEP) in France and Belgium.
This is the first genome-wide association study (GWAS) performed in alcohol-related HCC. It compared the genomes of thousands of individuals with alcohol-related liver disease with or without HCC.
This GWAS included more than 4,000 patients recruited from tertiary referral centers specialized in liver cancer screening and treatment in France and Belgium. The researchers identified an association between WNT3A-WNT9A genes and alcohol-related HCC.
The WNT3A-WNT9A genes are present in all individuals, however; there may be minor genetic variations amongst them. These are associated with a different risk of developing alcohol-related HCC.
Thus, in a population of chronic heavy drinkers, the study showed that 32% of individuals who had a protective variation in the WNT3A-WNT9A genes have a lower risk of developing alcohol-related HCC. In contrast, the 68% of patients who did not have the protective variation had an increased risk.
The researchers also confirmed that genetic variations in other genes (PNPLA3, TM6SF2 and HSD17B13) modulated the risk of alcohol-related CHC.
Hence, the simultaneous presence of deleterious genetic variations in the WNT3A-WNT9A, PNPLA3, TM6SF2, and HSD17B13 genes increases the risk of alcohol-related HCC.
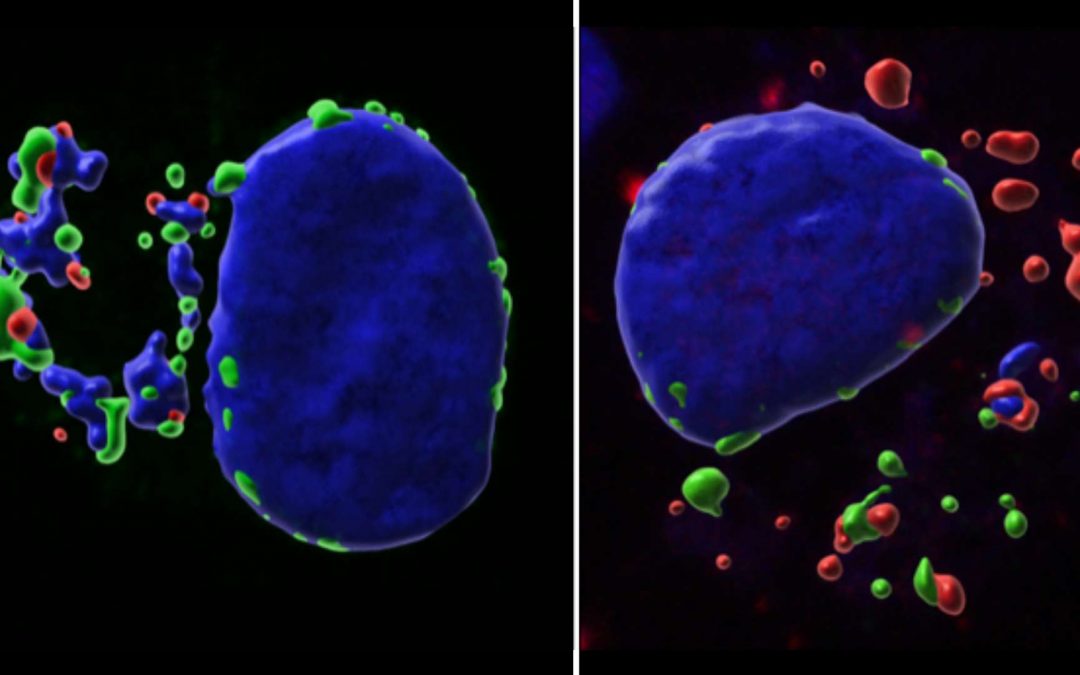
Lastly, the results of this study show that patients with alcohol-related HCC do not have the same tumor molecular characteristics depending on whether they carry the protective or deleterious genetic variations of the WNT3A-WNT9A genes. These common genetic variations may modify some well-known mechanisms involved in liver carcinogenesis. This study shows that these protective genetic variations may have an impact at a very early stage of hepatocarcinogenesis and may for example enhance immune system response and thus prevent the development of alcohol-related HCC.
This study contributes to a better understanding of the mechanisms associated with the development of alcohol-related HCC. It may also have unraveled a potential new therapeutic target against alcohol-related liver cancer. These results will also help the design of other studies, which will extensively assess the risk of developing alcohol-related HCC. In any event, it is important to highlight that limiting alcohol intake is the most impactful measure against the development of liver cancer irrespective of one’s genetic background.
This study was financially supported by the Ligue Nationale contre le Cancer (Labellisée Team), Bpifrance, Inserm (cancer plan), the Association Française pour l’Étude du Foie (French Association for the Study of the Liver), the Coup d’Élan of the Bettencourt-Schueller Foundation, the FRM Rosen Prize, the Ligue Contre le Cancer Comité de Paris (René and André Duquesne Prize), the Fondation Mérieux, and the Université Libre de Bruxelles in Belgium.
References
Common genetic variation in alcohol-related hepatocellular carcinoma: a case-control genome-wide association study – Eric Trépo, PhD *- Stefano Caruso, PhD *- Jie Yang, PhD *- Sandrine Imbeaud, PhD – Gabrielle Couchy, PhD – Quentin Bayard, PhD –
Eric Letouzé, PhD – Prof Nathalie Ganne-Carrié, PhD – Prof Christophe Moreno, PhD – Prof Abderrahim Oussalah, PhD – Prof Cyrille Féray, PhD – Prof Jean Frédéric Blanc, PhD – Prof Bruno Clément, PhD – Prof Patrick Hillon, PhD – Prof Jérôme Boursier, PhD – Prof Valérie Paradis, PhD – Prof Julien Calderaro, PhD – Viviane Gnemmi, PhD – Prof Jean-Charles Nault, PhD – Prof Jean-Louis Guéant, PhD
Prof Jacques Devière, PhD – Isabelle Archambeaud, MD – Carole Vitellius, PhD – Bruno Turlin, PhD – Prof Jean-Pierre Bronowicki, PhD – Prof Thierry Gustot, PhD – Angela Sutton, PhD – theGENTHEP Consortium † – Prof Marianne Ziol, PhD – Prof Pierre Nahon, PhD – Prof Jessica Zucman-Rossi, PhD
DOI : 10.1016/S1470-2045(21)00603-3
Research Contact
Prof Jessica ZUCMAN-ROSSI
PU-PH Université Paris Cité – Hôpital Européen Georges Pompidou (AP-HP)
Directrice du Centre de Recherche des Cordeliers – UMRS1138
jessica.zucman-rossi@inserm.fr
Read more
Theileria annulata and Cancer: a parasite strategy revealed!
A new study from Prof. Jonathan Weitzman’s research team at the Epigenetics and Cell Fate unit has shed light on the mechanism by which the parasite Theileria annulata, which causes a cancer-like diseases in cattle, evades the host cell’s defense mechanism.

Paris-Oxford Partnership (POP) Annonces its Results
The Paris-Oxford Partnership (POP) Evaluation Committee, composed of Université Paris Cité, CNRS, Institut des Etudes Avancées and Oxford University, announces the results of its calls for projects. The call aimed to facilitate and strengthen scientific collaborations...

Paris-Toronto Partnership launches its First Call for Proposals
Université Paris Cité and the University of Toronto are joining forces to launch their first call for proposals to support collaborative research initiatives. ObjectivesThe aim of the fund is to provide initial support for the development of research links and...
![[In Conversation] with Professors Anne Abeillé and Gabriela Bîlbîie](https://u-paris.fr/wp-content/uploads/2024/02/2024_PHOTOS-CHERCHEURES-1080x675.jpg)
[In Conversation] with Professors Anne Abeillé and Gabriela Bîlbîie
As part of Université Paris Cité's international guest researcher programme, Prof. Anne Abeillé is hosting Prof. Gabriela Bîlbîie, from the University of Bucharest in Romania. Our two professors are linguists specialising in theoretical and experimental syntax. We...
