Immunité innée et défense pulmonaire anti-infectieuse
This team is directed by Jean-Michel Sallenave, in the INSERM UMR1152 unit.
PRESENTATION
At the surface of the epithelium and pulmonary alveoli, epithelial cells and innate immune cells (alveolar macrophages, MDSCs, NK cells, Innate lymphoid cells/ILCs, eosinophils..) interact, through the production of surfactant, regulatory cytokines and antimicrobial molecules, to ensure a non- inflammatory regulatory phenotype.
After infective or toxic stimuli exposure, these cells participate in a network to organize pro-inflammatory responses and to engage adaptive immunity to contain the aggression, foster tissue repair, and to insure the return to haemostasis.
Our research group (Team 3, INSERM U1152, Faculté de Médecine, Hôpital Bichat, Paris) is mostly interested in the innate mechanisms put in place in these processes and in the dysregulation of these control mechanisms.
Relatedly, we have a keen interest in translational medicine since a dysregulation of these control mechanisms could potentially explain the pathophysiology of some inflammatory disorders (chronic obstructive pulmonary diseases/COPD, cystic fibrosis, ventilator-associated pneumonia..)
Four main areas of investigation are currently being pursued in our team :
1) Study in vitro and in vivo of the role of Pseudomonas aeruginosa infections (an opportunistic pathogen in pulmonary nosocomial infection and in cystic fibrosis) in exacerbations of chronic lung diseases, including cystic fibrosis.
2) In vitro and in vivo study of the mechanisms through which Influenza virus, a pathogen responsible for lung infections in seasonal flu or pandemic episodes can favour bacterial super-infections and induce disease exacerbations in chronic lung diseases.
3) Study of host-pathogen interactions in COVID-19
4) Investigation of the molecular mechanisms of action of nanoparticles in the lung, in isolation or in conjunction with lung pathogens (S. aureus, P.aeruginosa, Influenza virus…), and their use as potential adjuvants in vaccination protocols.
Technological tools : the molecular processes, techniques, reagents, signalling pathways studied and used in this context include :
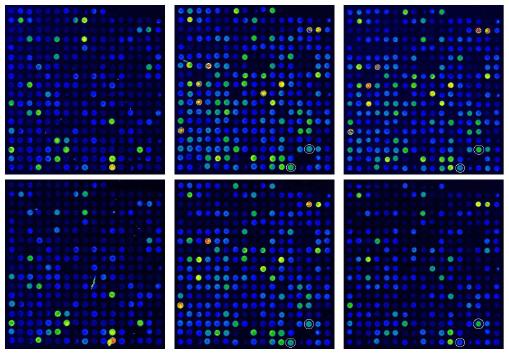
-mechanisms of Pathogen Associate Molecular Pattern/PAMP receptors activation, phagocytic processes, signal transduction pathways ; role of epithelial type 2 serine proteases (TTSPs) during Influenza infection ; interactions between microbial virulence factors, innate immune receptors and epithelial channels (eg CFTR) ; study of endogenous antimicrobial molécules ; use of recombinant adenovirus vectors in over-expression protocols ; in vivo rodent infection models ; RT-qPCR ; flow cytometry ; immuno-histochemistry ; proteomics.
Recent Selected publications
-Saint-Criq V et al. Thorax, 2018; 73:49-61 ; -Villeret B et al. ACS Nano. 2018;12:1188-1202 ; -Bastaert F et al. Front Immunol. 2018;9:1675. ; -Sanchez-Guzman D et al. Biomaterials. 2019;217:119308 ; -Villeret B et al. Front Immunol. 2020, 11:117 ; -Sallenave JM, Guillot L. Front Immunol. 2020;11:1229 ; -Kheir S et al. BioRxiv preprint : https://doi.org/10.1101/2020.07.22.214684
Current Research Funding :
-
Vaincre la Mucoviscidose :
-Etude du statut des lymphocytes innés ILCs dans le tractus respiratoire des patients mucoviscidosiques : analyse et mécanismes physio-pathologiques »
-Etude de la voie IL-6/antimicrobiens/réparation dans la mucoviscidose : étude mécanistique et interventionnelle
-
– Université Paris Cité : « Fonds d’urgence en soutien aux unités de recherche mobilisées sur le front du SARS-Cov-2 et du COVID-19 »
-
-Carb-X : (‘Combating antibiotic resistance bacteria’, Boston, Wellcome Trust, Bill and Melinda Gates)
-
-ANR : ‘Muc-Vac’ : Administration in situ d’IL-7 comme adjuvant de vaccination muqueuse
-
-ANR : Franco-Allemande : Résistance anti- microbienne
-
-FRM : Contribution de la pollution atmosphérique particulaire dans la sévérité de l’infection par le virus de la grippe
