Alexandre Loupy, professor at Université Paris-Cité (AP-HP/Université Paris Cité), nephrologist at the Necker Children’s Hospital, is one of the two winners awarded the prize for Innovators in Health from the Ile-de-France region.
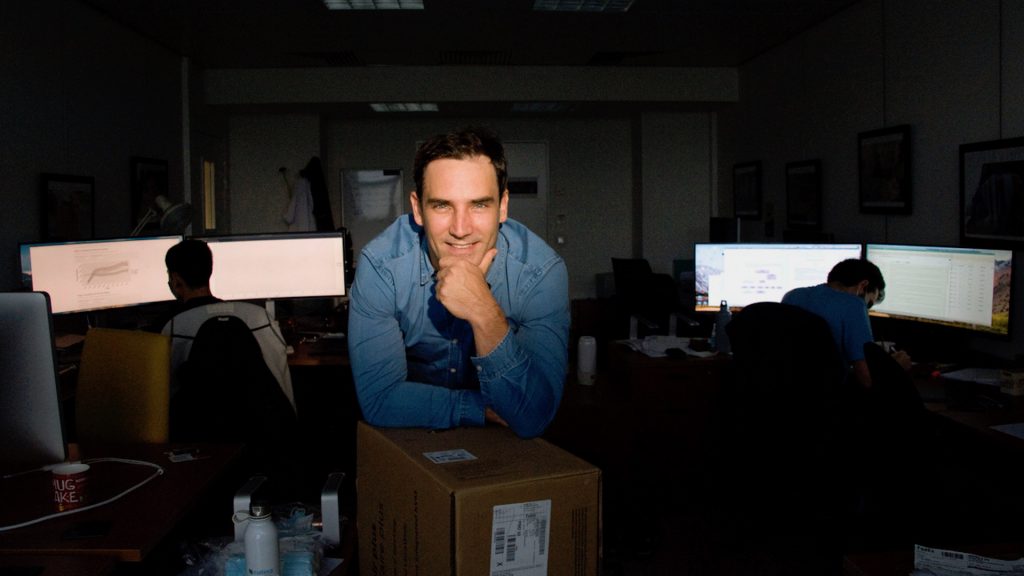
Alexandre Loupy received 25,000 euros for his discoveries in transplantation and graft rejection, as well as for the implementation of an application based on artificial intelligence. The iBox will enable to evaluate during each patient visit, the probability of renal graft survival, based on the biological, immunological and histological data available at the time of the consultation.
Can you tell us about your project? How does artificial intelligence contribute to significant developments in your field of research?
Renal transplantation is currently recognised as the best treatment for end-stage renal failure, by improving quality of liefe and lifespan while substantially reducing costs for society. However, despite the progress made, allograft rejection remains a major cause of graft loss and has a major economic impact for the healthcare system.
To meet these requirements, over the past 15 years at the Paris Transplant Group, we have developed a prospective cohort of kidney transplant patients, offering a unique level of phenotypic detail as it combines clinical, biological, immunological, phenotypic, histological and transcriptomic data, as well as applied biostatistics. The vast amount of information retrieved from several thousand patients longitudinally results in an integrative and translational “smart data” approach, harnessed by artificial intelligence. In 2019, this initiative led to the development of an algorithm for individual prediction of the risk of rejection and graft loss, generated by algorithmic analysis of over 85 peri- and post-transplant parameters.
This prognostic system enables us to predict in a very reliable way, soon after transplantation, the outcome of a patient’s transplant over the next 10 years. This algorithm has been approved in 12 centers in Europe and the United States, as well as in 3 international randomized trials. The lead article was published in 2019 in the BMJ journal. In the same year, this discovery was awarded a prize by the Academy of Medicine and in 2020 by the American Histocompatibility Society. The iBox system, integrates all the relevant demographic, functional, histological and immunological factors measured in routine clinical practice, as well as all the therapeutic, diagnostic and technical advances made in recent years. It also illustrates the potential of the approach developed by our team, including sound statistical methodology applied to multidimensional population data, to deliver concrete results on rejection mechanisms, risk stratification and optimized, personalized patient follow-up.
What societal and medical impact will your work have on public health?
The results generated by the iBox system will provide physicians with information on the functional status of the graft and the different trajectories of functional decline, enabling them to adapt patient follow-up and assess response to treatment. For example, iBox will enable early detection of the consequences of therapeutic changes on long-term kidney graft survival.
The iBox will also contribute to changing the evidence base for clinical trials, by bringing a new generation of clinical trials into practice with the prognostic system. In June, iBox officially entered the qualification process as a “surrogate end point”, enabling therapeutic trials in transplantation to be reduced by 7 years, since the final judgment criterion corresponding to rejection and organ loss can be substituted for the early evaluation of the iBox score. This therefore offers a major opportunity not only for improving patient care, but also for therapeutic innovation, which is currently limited by the long duration of clinical trials.
What does this award mean to you, and how do you intend to use it in the future?
The goal of our team’s work is to apply the concrete scientific discoveries we have made over the last 5 years to everyday clinical practice. This translation of research “to the patient’s bedside” is a major motivating factor. On the other hand, transplantation medicine is a complex, demanding, multidisciplinary field involving many medical and paramedical professionals. Added to this is the increasing phenotypic complexity of patients’ clinical pictures, with the implementation of biomarkers and transcriptomic tools in daily patient assessment.
This complexity is conducive to the implementation of algorithmic tools designed to use the most relevant medical data for patient follow-up, and to facilitate and guide medical decision-making. The funds requested by this application will enable us to develop the iBox system by adding functionality to standardise care practices. We propose to implement a clinical and care protocol functionality in the iBox application. It will take the form of decision-making models based on clinical profiles and specific situations. This tool for practitioners will be an additional support to medical decision-making, and will reinforce the clinical usefulness of iBox by standardising care practices.
Read more
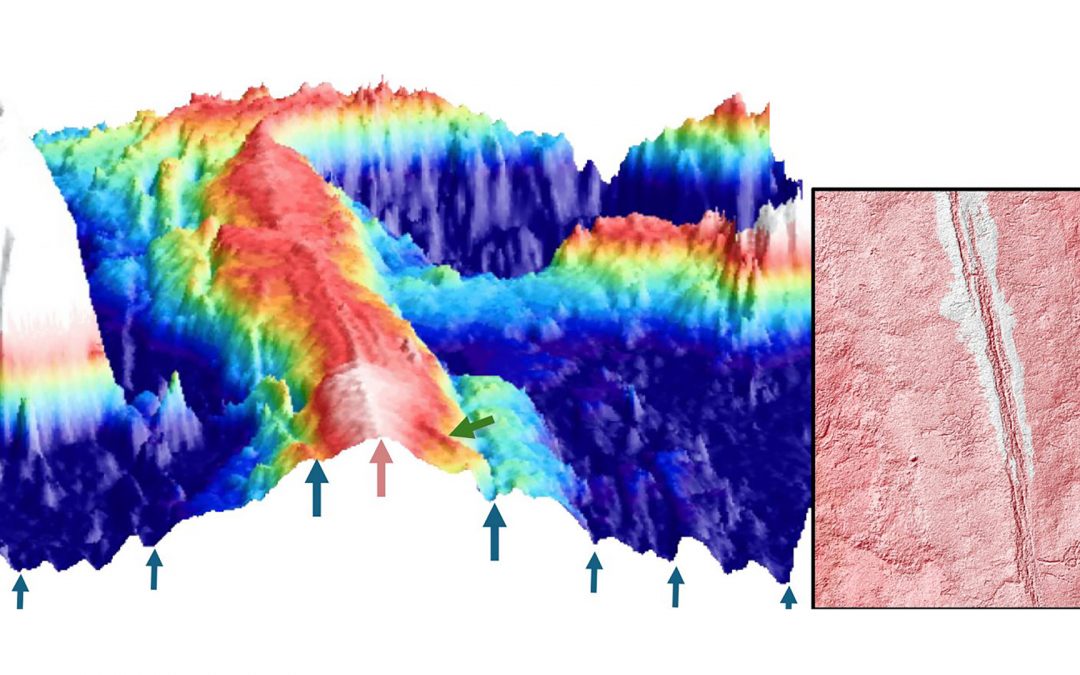
Evidence of magmatically induced faults at the East Pacific Rise
By comparison of ultra-high-resolution 3-D seismic imagery and bathymetry data collected at the East Pacific Rise (EPR) 9º50'N, researchers reveal the existence of magmatic induced faults near the ridge axis.
read more
Convergences: A Strategic Alliance paving the Future of Biology-Health Research
A key milestone for the partnership between Institut Pasteur and Université Paris Cité, the first “Convergences” scientific seminar took place on June 17th at the university’s head office at Odéon.
read more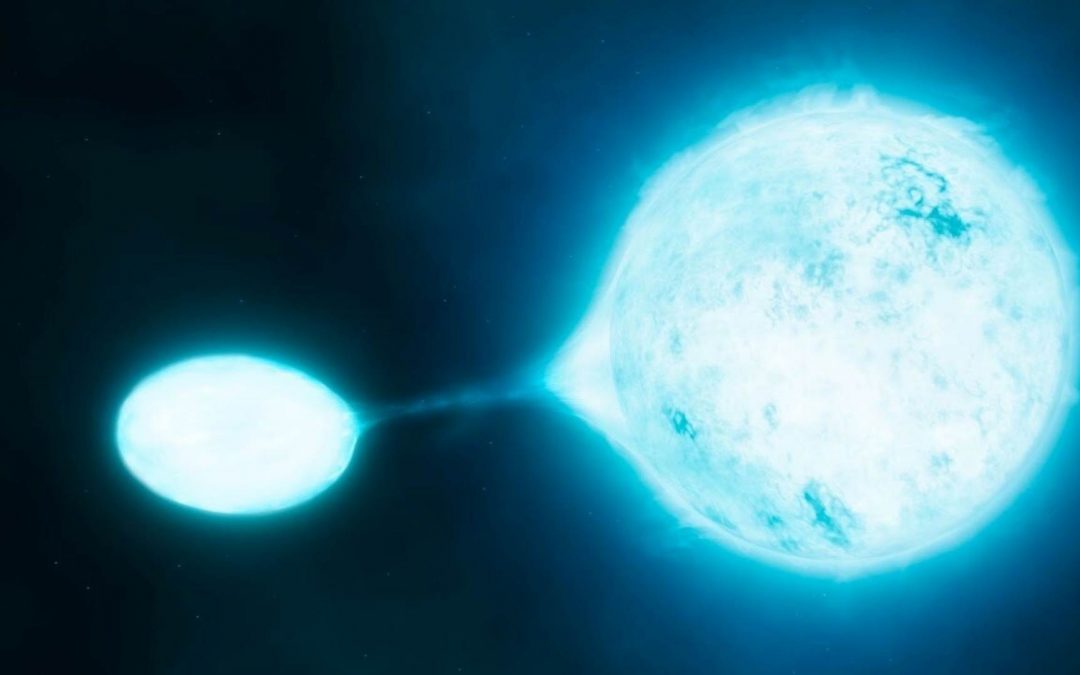
Université Paris Cité receives 2 grants from Marie Sklodowska Curie Actions programme !
The results of the MSCA Staff Exchange 2023 call for proposals were published on May 28 2024. Université Paris Cité congratulates its two winners, Sylvain Chaty, Professor and Vice President for Culture, Science and Society at the AstroParticle and Cosmology...
read more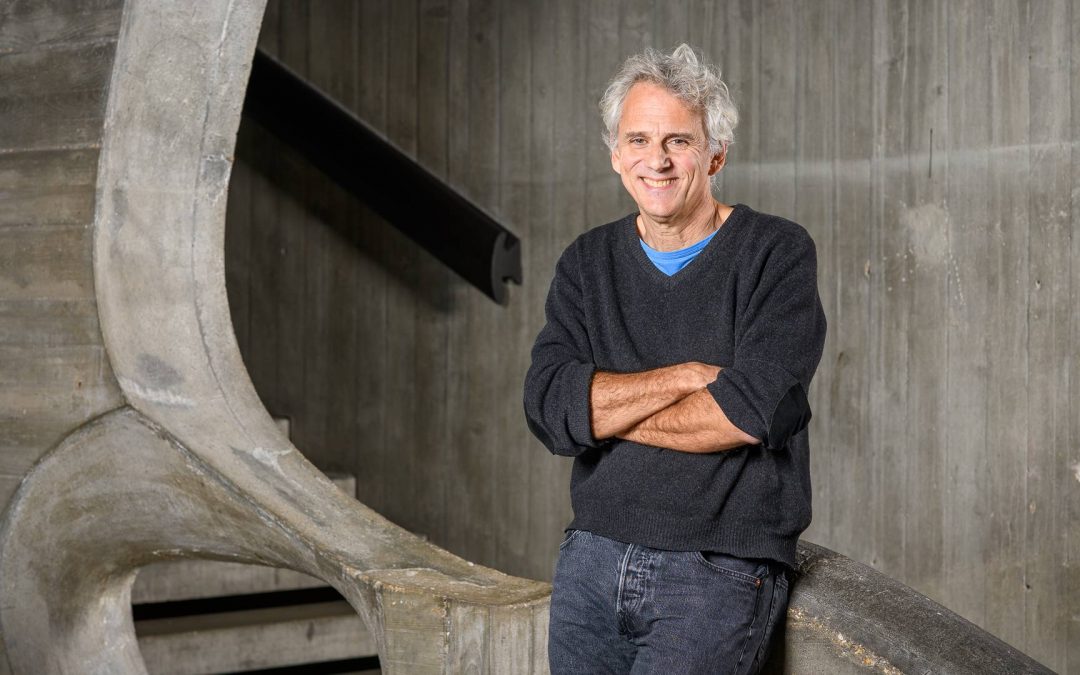
MENTOR: Winner of the MSCA Doctoral Networks 2023
When abnormally activated, the mTOR protein can contribute to the development of cancers and certain monogenic diseases that affect around 2 million people worldwide. The multi-disciplinary MENTOR project, which stands for Metabolic control of cell growth by mTOR in...
read more